I have discussed my cirrhosis diagnosis quite a bit. It has been educational and stressful, all at the same time. I try to share what I have learned as educational but not a blueprint for anyone else. It is a disease that doctors are still learning about, thankfully, mine admits that there is a lot of information they simply do not know. That doesn’t always offer hope, as a patient. I sometimes wished that there was a cirrhosis primer out there for all newly diagnosed patients. My hope is that my journey may help alleviate some of your fears, if you have been recently diagnosed. One of the things that seems to cause a lot of confusion is the MELD score and what it means.
As a cirrhosis patient, I understand the weight of uncertainty a diagnosis can carry. The Model for End-Stage Liver Disease (MELD) score is a tool we use to assess the severity of your condition and guide treatment decisions. In this article, we’ll delve into what a MELD score is, how it’s calculated, and how you can be an active participant in managing it.
- MELD and Cirrhosis: A Numbers Game
- Blood Tests: The Building Blocks of a MELD Score
- Beyond the MELD Score: Regular Blood Tests for Cirrhosis Upkeep
- Taking Charge: Managing Your MELD Score
- Beyond Blood Tests: Other Factors Affecting MELD
- Working Together for Your Well-Being
MELD and Cirrhosis: A Numbers Game
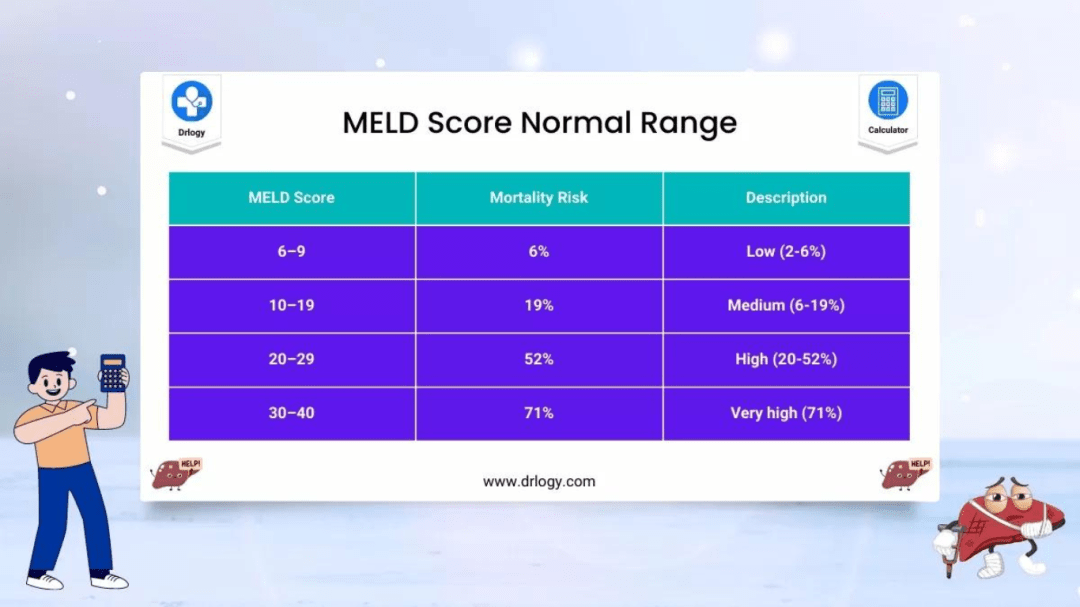
Cirrhosis, a condition where healthy liver tissue is replaced by scar tissue, can significantly impact liver function. The MELD score is a numerical representation of this impact, ranging from 6 (least severe) to 40 (most severe). However, the MELD score isn’t just a single number – different score ranges point to potential issues that may arise as cirrhosis progresses:
- Lower Scores (6-10): This range indicates relatively well-preserved liver function. While complications are still possible, the risk is lower.
- Intermediate Scores (11-20): As the score climbs, the risk of complications like fluid buildup in the abdomen (ascites), variceal bleeding (bleeding from enlarged veins in the esophagus or stomach), and hepatic encephalopathy (confusion due to liver dysfunction) increases.
- Higher Scores (21-40): Scores in this range indicate significant liver dysfunction. The risk of serious complications and mortality rises considerably. Patients with scores in this range are often prioritized for liver transplant evaluation.
It’s important to remember that the MELD score is a tool for prediction, not a guarantee. However, understanding how your score relates to potential complications empowers you and your doctor to make informed decisions about treatment and monitoring.
Blood Tests: The Building Blocks of a MELD Score
The MELD score relies on three readily available blood tests to paint a picture of your liver function. These tests act as the building blocks, with each value plugged into a formula to generate your final score. Let’s delve into these three tests and understand how they reflect the health of your liver and contribute to your overall MELD score.
Three routine blood tests form the foundation of your MELD score:
- ** Bilirubin:** This yellow pigment, a byproduct of red blood cell breakdown, rises when your liver struggles to remove it.
- ** INR (International Normalized Ratio):** This test measures how well your blood clots, reflecting how impaired your liver function is.
- ** Creatinine:** This waste product, normally eliminated by the kidneys, can rise when your liver function declines and affects kidney function indirectly.
By factoring in the values of these tests, a formula generates your MELD score. The higher the values of bilirubin and INR, and the lower the creatinine level, the higher your MELD score.
Beyond the MELD Score: Regular Blood Tests for Cirrhosis Upkeep
In addition to the blood tests used in the MELD score calculation, regular blood tests are crucial for monitoring your overall health and identifying potential complications of cirrhosis. These tests may include:
- Complete Blood Count (CBC): This test evaluates your red and white blood cells and platelets, providing information about potential anemia, infection risk, and bleeding risk, respectively.
- Liver Function Tests (LFTs): This broader panel includes additional enzymes and proteins besides bilirubin that can offer a more comprehensive picture of your liver function.
- Viral Hepatitis Testing: If viral hepatitis contributed to your cirrhosis, regular testing is needed to monitor the viral activity and guide treatment decisions.
- Electrolytes: These minerals are essential for various bodily functions, and imbalances can occur in cirrhosis.
By following a regular blood testing schedule, we can proactively manage your cirrhosis, identify complications early,and adjust treatment plans as needed.

Taking Charge: Managing Your MELD Score
A MELD score provides valuable insight into your liver function, but it’s important to understand that certain aspects of the score, like the core blood tests used in the calculation, are not directly modifiable. However, this doesn’t mean you’re powerless to influence your MELD score and overall health. By focusing on aspects you can control, like diet and adherence to medications, you can become an active participant in managing your cirrhosis and potentially improve your MELD score. This proactive approach can empower you to cope with your condition and take charge of your well-being.Let’s explore some lifestyle changes and treatment strategies that can positively impact your MELD score and quality of life.
While the core blood tests cannot be directly altered, some lifestyle changes can indirectly influence your MELD score:
- Diet: Maintaining a healthy weight and avoiding excess salt can reduce stress on your liver.
- Medications: Following your doctor’s prescribed medications for cirrhosis and other conditions can improve your overall health.
- Abstinence from Alcohol: If alcohol abuse contributed to your cirrhosis, complete abstinence is crucial.
- Treating Underlying Conditions: Addressing conditions like hepatitis can improve liver function.
Beyond Blood Tests: Other Factors Affecting MELD
The MELD score, while a powerful tool, primarily focuses on the information gleaned from blood tests. However,cirrhosis is a complex condition that can manifest in various ways. This section will explore other factors beyond the blood work that can influence your overall health and potentially impact your MELD score indirectly. These factors can provide a more comprehensive picture of your condition and help us tailor treatment plans to address your specific needs.
Other factors that can affect your MELD score include:
- Presence of Ascites (fluid buildup in the abdomen): This complication of cirrhosis can worsen your prognosis.
- Hepatic Encephalopathy (confusion due to liver dysfunction): This can indicate a more severe stage of cirrhosis.
- Nutritional Deficiencies: Poor nutrition can further compromise your liver function.
Working Together for Your Well-Being
A MELD score is a valuable tool, but it’s just one piece of the puzzle. Doctors will consider your overall health, including the factors mentioned above, when making treatment decisions. Open communication and adherence to treatment plans are crucial. By working together, you can manage your cirrhosis and explore options to improve your MELD score and overall well-being. Remember, this article provides general information. Always consult your doctor for personalized advice and to discuss your specific MELD score and its implications.
I hope this article offers you some insightful information, but please remember that I am not a doctor and my info won’t, while helpful, may not be the best for you. Consult your doctor and tell them any concerns you have or anything that may be bugging you, it is your life, after all. Let me know in the comments below if you found this information useful. If you have been recently or even been dealing with cirrhosis for a while, let me know in the comments, also. Your information may help others feel more safe than they do at this very moment.